As my friends have gotten older, more of them have started to experience some level of hearing loss, so occasionally someone asks me for advice, and it occurred to me that I could make a post here that I can just point people to when they ask.
Before I get to that, I should add a disclaimer: I am neither a doctor nor an audiologist or any kind of medical professional, and this post is based solely on my personal experiences with hearing loss. If you have any questions about your own hearing, please consult an ENT or an audiologist.
I will also mention that while some of this advice may be applicable to parents of children with hearing loss, I am a late-deafened adult with no kids. Therefore, I have no experience in handling hearing loss as a child, or as a parent of a deaf or hard-of-hearing child. Obviously, learning to sign is an option for anyone who loses their hearing, but as I have not done it, it’s also not a subject I have any experience in. This post is mainly aimed at late-deafened adults who have lived all their lives in the hearing world and want to stay there, although it is of course a perfectly valid choice to join the Deaf community and communicate exclusively by signing.
Specific bits of advice will be in bold and italics, in case you want to skip to them.
Sudden Hearing Loss
A lot of times, hearing loss happens to older people and comes on gradually — this is why there’s such a stigma around it, because it’s seen as an “old people’s problem.” However, as I personally can attest, sometimes even young people can lose hearing very suddenly and for no apparent reason.
If you experience a sudden loss of hearing, go see an otolaryngologist (ENT) as soon as possible. I cannot stress this one enough! If you call and they can’t get you in for weeks, push back or try someone else, because sudden hearing loss is an emergency, and the longer you wait for treatment, the less likely it is to work.
Treatment for sudden hearing loss usually involves a course of steroids, either oral or injected directly into the eardrum or both. They don’t always work, and even if they do, you may still end up with some level of loss, even if it’s not as severe as it was initially. So again, it’s extremely important to get to a doctor as soon as possible, preferably within a day or two after you notice the loss.
The ENT may also recommend an MRI after a sudden loss of hearing, in order to determine if there are any tumors that could be causing the loss.
Getting a Hearing Test
The first thing anyone with hearing loss needs to do is find a good audiologist and get a hearing test. I don’t really have advice on finding an audiologist besides the standard stuff, like looking at reviews and getting recommendations from your doctor. (Many ENTs will have audiologists on staff, so often you can just see theirs if you’ve also gone to a doctor.)
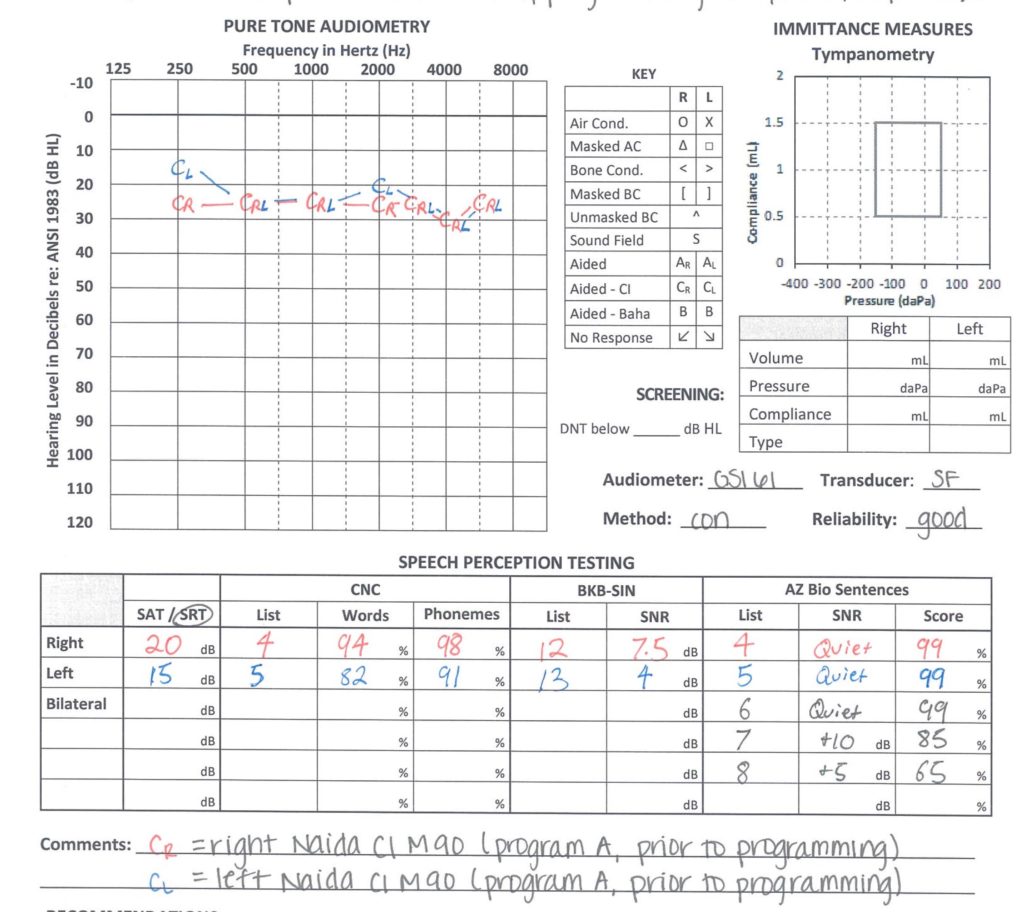
Hearing tests typically have a couple of parts. The first is called “pure-tone audiometry”. This is where they play you a series of beeps and you press a button or raise your hand when you hear them. The tones will usually start out loud and then get softer, or vice versa; the object here is to see how loud a sound needs to be before you can hear it. The louder it needs to be, the more pronounced your hearing loss is. Some hearing loss occurs only at specific frequencies; for example, you might have trouble with the higher ones but be fine in the lower range. After this test, the audiologist will produce an audiogram representing your specific hearing levels.
I won’t go into how to read an audiogram here; there are plenty of resources for that, like this: https://www.healthyhearing.com/report/52516-The-abc-s-of-audiograms
The second part of a hearing test is word recognition. Either the audiologist or a recorded voice will say words and you have to repeat them back. More thorough tests might even include sentences or background noise. They will probably test each ear separately, and assign a word recognition score (WRS) at the end, which is the percentage of words you heard correctly.
Always ask for a copy of your audiogram for your own records. If your hearing loss should progress, having this history will be helpful to future doctors and audiologists. I did not do this at first, and was chided by several doctors who wanted to know how my hearing had changed over the years.
Hearing Aids
If you do have hearing loss (but aren’t totally deaf), the next step might be to get a hearing aid. Hearing aids are basically little amplifiers. Microphones on the outside pick up the sounds around you and send it to a little speaker in your ear canal. Therefore, hearing aids may not help if your hearing loss is severe, because they only amplify sound, meaning you have to have some hearing in order for them to be effective.
There are several types of hearing aids available; this page does a pretty good job of listing several of them: https://www.healthyhearing.com/help/hearing-aids/types
Your audiologist is the best one to assess your specific hearing loss and recommend which type of hearing aid might be best for you.
The most important piece of advice I have for people who are looking for hearing aids:
Before you pay them a dime, make absolutely sure that you get a trial period of at least a month, more if possible. This will allow you to try out the new hearing aids in the real world and see how well they work for you, because when you’re sitting in the audiologist’s quiet office and it’s just you and them, that’s not a really good example of the situations you will encounter in daily life.
Most US states have laws requiring a trial period for hearing aids; I don’t know about other countries. Always, always ask the audiologist about this before you buy, because you should absolutely be able to get your money back if they don’t work for you. (I got burned the first time out and was stuck with a useless HA, because I wasn’t aware of this.)
Once you have your hearing aids, make the most of your trial period by using them in a variety of situations. How well you hear in a quiet room is going to be different from a crowded restaurant, or a live concert, or a movie theater, so you will want to try out as many of these settings as possible.
Keep notes on how well you’re hearing in different situations. With most modern HAs, the audiologist can give you different programs for different situations, or tweak your existing ones. Just because it doesn’t work for you at first doesn’t mean it can’t be adjusted; modern HAs have some pretty sophisticated abilities to handle specific types of hearing loss and specific settings (like lots of background noise). You might need to see your audiologist a couple of times during the trial period; however, if you get to the end and you’re not happy, don’t hesitate to return it and ask about other options.
Once you settle on a hearing aid you like, go see the audiologist at least once a year, or however often they recommend. Your hearing may change over time, so once you start losing it, it’s a good idea to get regular tests, talk to the audiologist, and have them make any necessary adjustments.
Volume and clarity are two very different things. This is something a lot of people who have never had hearing loss don’t really understand, and it’s also why hearing tests include both tones and word recognition. When I got my first HA for my left ear, it made everything louder, often to the point where things were way too loud. However, if I covered my good ear and just tried to listen with the HA in the other ear, it sounded like the other person was speaking through a pillow: the words were loud enough, but I couldn’t make them out, and my word-recognition score in that ear, even with a hearing aid, was somewhere around 10%. Conventional hearing aids can help with volume, but they do nothing for clarity, so there may come a point where they’re not useful.
Different hearing aids have different capabilities and accessories. If Bluetooth streaming is important to you, ask the audiologist before they order your HAs, as some do have the ability to stream built in. Some also have phone apps to allow you to tweak certain settings on the fly. Not all of them can do these things, so it’s important to tell the audiologist what’s important to you.
No two people’s hearing loss is the same, so what works for someone else may or may not work for you. This is why I am avoiding making any specific brand recommendations here. The only way to know what will work for you is to see an audiologist and try some out.
Single-Sided Hearing Loss
Some people only lose hearing on one side, and the other is fine. If a conventional hearing aid works on the bad side, great! But if it doesn’t, ask your audiologist about CROS hearing aids. These come in pairs; one goes in your bad ear and has the usual microphones to pick up sound, but instead of the sound going into the same ear like with conventional HAs, the one in the bad ear acts as a transmitter, which sends the sound from the bad side into a receiver in your good ear. This allows you to hear sounds on both sides through the same ear.
There is also a related type called BiCROS, which is for people with severe to profound hearing loss in one ear and mild to moderate loss in the other. They’re basically the same as CROS, except that the good side also has amplification in addition to being a receiver for the bad side.
CROS/BiCROS HAs aren’t for everyone; like everything, they have their advantages and disadvantages. Again, this is why a trial period is so important.
Surgical Options
There may come a time when conventional hearing aids don’t cut it (see above point about volume vs. clarity). We are pretty fortunate to be living in an era where some pretty amazing medical technology exists that can help. This is obviously something you’d want to discuss with your ENT if an audiologist says your hearing has deteriorated past the point where HAs can help, but I’ll mention a couple of options here.
The first is a BAHA, or bone-anchored hearing aid. They are surgically implanted; you can find info about them on the web (for example: https://www.hopkinsmedicine.org/otolaryngology/specialty_areas/hearing/hearing-aids/baha.html). You can actually try one of these without the surgery; my ENT lent me one to try some years back. (Without the surgery, a headband holds it in place.) BAHAs are used to bypass the outer and middle ear, so they’re only useful for certain types of hearing loss.
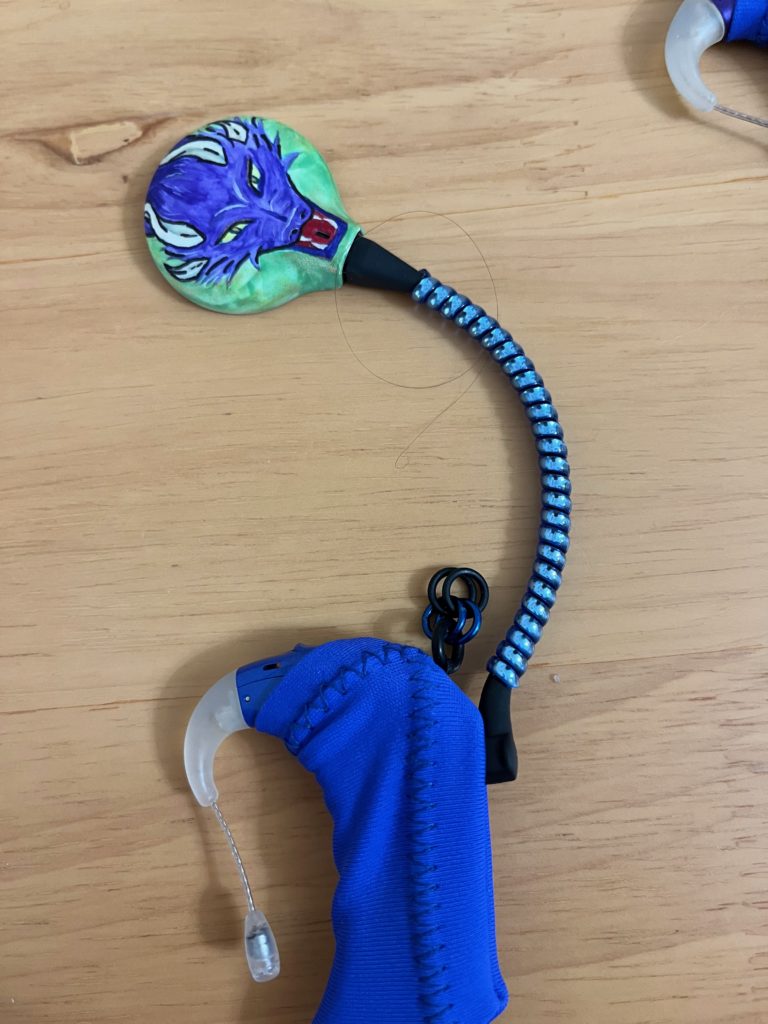
And the second, of course, is cochlear implants, which can be an option for people with severe to profound hearing loss when hearing aids no longer work. If you read the rest of this blog, you can find out how I ended up with them, from the evaluation process on up through surgery and activation, so I won’t go into that story here. The one thing I will say on this catchall page is: Neither CIs nor HAs are perfect. Once you start experiencing hearing loss, you will never have your normal hearing back again exactly as it was before, and it’s depressing to keep dwelling on that fact. I do my best to try and remember that it’s better to compare my current level of hearing with what I would have if this technology didn’t exist, rather than with the way my hearing was before I needed it, because my normal hearing is not coming back. So even though I do still have my struggles, I am incredibly grateful that I’m living in an age where this technology has been able to restore my hearing — not to normal, but to good enough to function in the hearing world.
Other Accommodations
People new to hearing loss may not be aware that accommodations do exist, although you often have to ask for them. Some movie theaters offer open-captioned showings at selected times, where the captions are displayed right on the screen. For those who live in the greater Washington, DC area, there is a group that organizes OC screenings in DC, Maryland, and Northern Virginia; you can find them on Facebook: https://www.facebook.com/groups/974135299310973
Movie theaters will also provide captioning devices if you ask, but I personally dislike them and prefer to seek out OC screenings. And the larger live theaters will also often have open-captioned shows; just look for “Accessibility” on their web page or call them and ask.
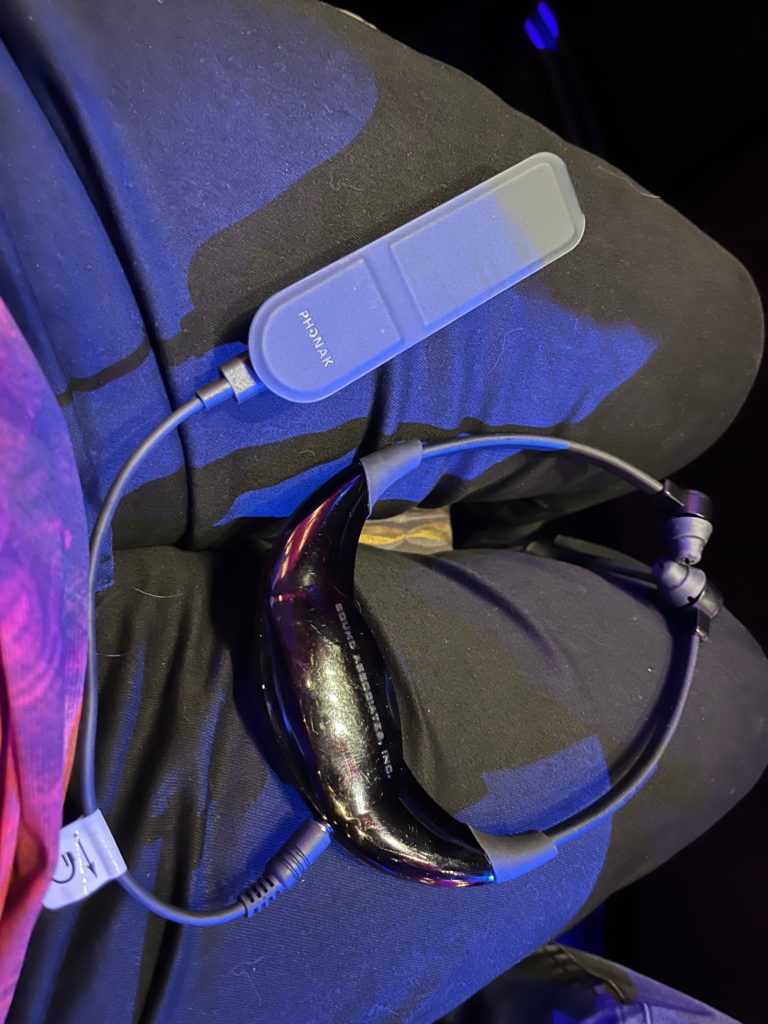
In addition, many theaters (both movie and live) also offer assisted listening devices (ALDs), though again you have to know to ask for it. These are small FM receivers with headphones, so you can get the movie or show’s sound directly from the theater’s sound system, which can be helpful if you have trouble hearing it through the theater’s speakers. I actually have an accessory that I can plug into an ALD’s headphone jack, which will stream the sound directly to my CIs, which is really nice. I can hear the movie sound okay just with the speakers, but it’s always clearer if I can stream it. This also has the additional benefit of blocking out any sound from the rest of the audience, so you can’t hear babies crying or people coughing or talking.
All modern hearing aids and CIs also have telecoils. This is an older technology that uses electromagnetic signals to transmit sound. It’s not hugely common in the US, but I know of at least one live theater (the Kennedy Center in DC) that offers ALDs with optional neck loops that transmit to t-coil HAs and CIs. You can also buy a neck loop which can be plugged into any device’s standard headphone jack and will transmit the device’s sound to your t-coil. However, this functionality must be enabled in your HA or CI by an audiologist in order to use it.
There are also live-captioning apps for various phones which will display speech on the screen. In a pinch, the Notes app which comes standard on Apple’s iPhone can be used to transcribe speech in real time; just open it up and tap the little microphone, and any words it picks up will show up on the screen. These apps are not perfect, but they can be helpful. Zoom, MS Teams, and other meeting apps also will often have a live-captioning option; you just have to look for it.